A 60 year old female with vomitings and loose stools since 2 months
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CONSENT WAS GIVEN BY BOTH PATIENT AND ATTENDERS
A 60 year old female, presented to the OPD with chief complaints of :
- vomitings and loose stools since 2 months
- generalised weakness since 20 days
History of Presenting Illness : The patient was apparently asymptomatic 2 months ago, then she developed vomitings, 5-6 episodes per day with food material as content, non bilious, non projectile, non blood stained releived with medications.
Complaint of loose stools since 2 months, 4-5 episodes per day, large volume, watery, non foul smelling, non blood stained releived with medications.
Complaint of joint pains since 20 years, first of the small joints of the foot and ankle, then the knees and then joints of the hands, wrist, elbow and shoulder joints .
Patient had undergone total knee replacement surgery for the right leg 8 yrs back and for the left leg 4 yrs back.
Pt has complaint of dry mouth and dry eyes since 20 yrs.
Complaint of itching of lower limbs and upper limbs since 4 yrs .
Complaint of loss of vision of left eye since 18-20 yrs and blurring of vision of right eye since 2 yrs.
Patient was diagnosed with hypothyroidism 20 years back when the pt had undergone a general checkup for weight gain and hair loss.
Pt is now using 75 mcg THYRONORM .
Patient was diagnosed with hypertension 1 year back on regular checkup, now using ATEN 25 mg PO/OD.
Past History :
Pt has history of Rheumatoid Arthritis since 20 yrs.
Pt has history of hypothyroidism since 20 yrs using 75 mcg THYRONORM.
Pt has history of hypertension since 1 year on ATEN 25 mg PO/OD.
History of hysterectomy surgery done 20 yrs back.
Not a known case of diabetes mellitus, epilepsy, asthma, CAD .
Personal history :
Diet - vegetarian
Appetite - decreased since 2 months
Sleep - adequate
Bowel and bladder movements - regular
Addictions - none
Family history : not significant
General Examination : The patient is conscious, coherent and cooperative . She is moderately built and nourished .
Pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy, peripheral edema - absent.
Bed sores
Systemic Examination :
CVS : S1, S2 heard. No murmurs.
RS : BAE present. NVBS heard.
CNS : No focal neurological deficits. Higher mental functions intact.
P/A : soft, no organomegaly.
Tenderness present at the supra pubic region.
Investigations :
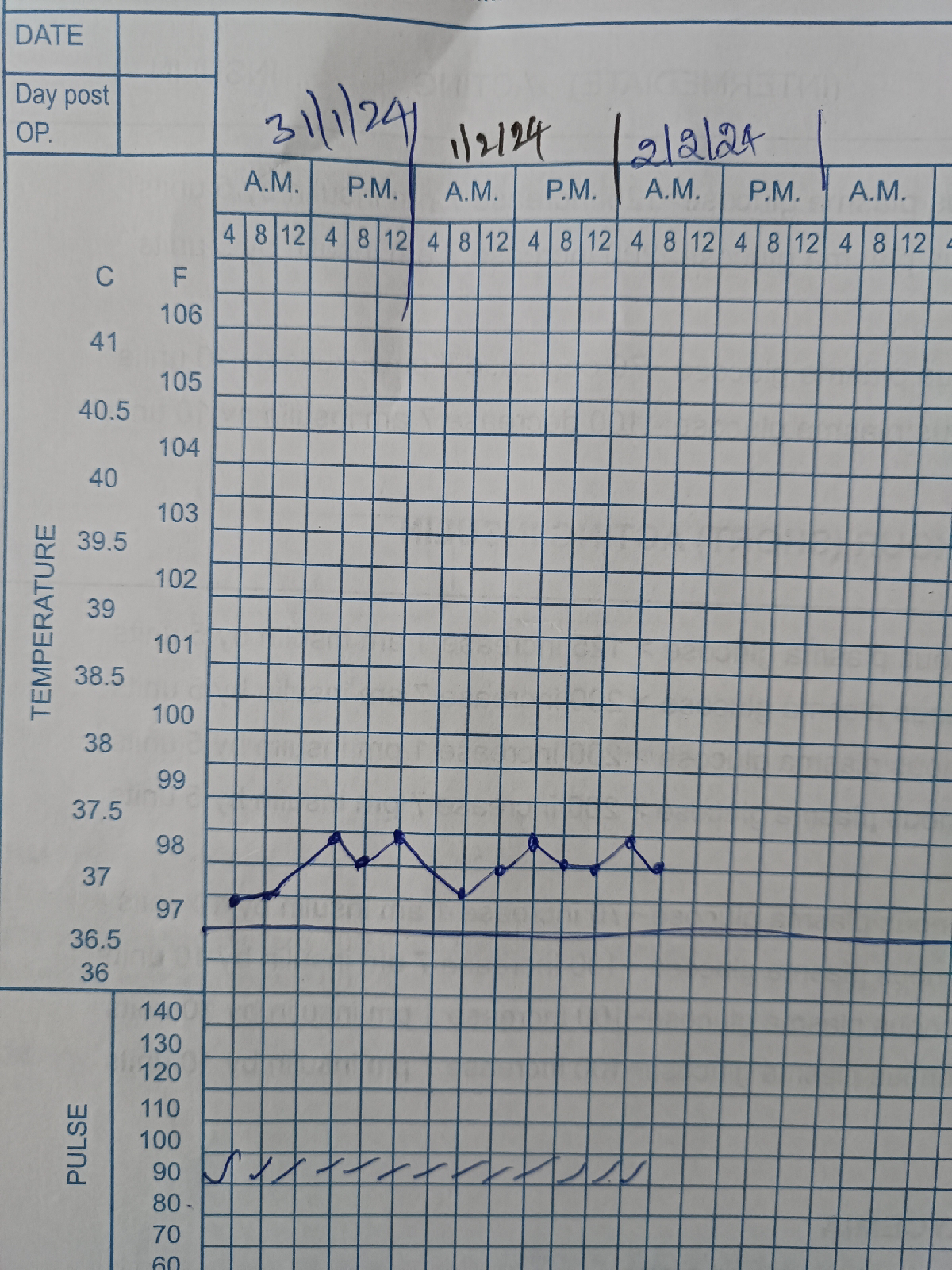
30/01 01/02
Hb 8.1 7.1
RBC 2.96 2.62
Urea 44 24
Creatinine 2.5 2.1
Uric acid 9.2 8.4
Sodium 135 138
Potassium 3.2 3.5
Chloride 102 105
RBS - 111 mg/dl
T3 - 0.55
T4 - 16.30
TSH - 8.57
Serum iron - 74
Serum ferritin - 198.3
Diagnosis : Gastroenteritis
K/C/O Rheumatoid Arthritis with
Secondary Sjogren 's syndrome with
Senile Xerosis with
Anemic Pruritis with Anemia of Chronic Disease with
Hypertension with
Hypothyroidism with
AKI on CKD with
Left eye Anterior Staphyloma
Right eye Keratoconjunctivitis Sicca with
Grade 2 and 3 Bed sores
Treatment :
Inj. ZOFER 4 mg IV/TID
Inj. PAN 40 mg IV/OD
Tab. THYRONORM 75 mcg po/od
Tab. OROFER po/od
Tab. TECZINE 10 mg po/od
Liquid paraffin L/A BD
Fucidic cream L/A BD
Lubrex eye drops 4 times/day
Tab. SPOROLAC DS SOS

























Comments
Post a Comment